A Generational Opportunity for Rural Healthcare
At a time when rural healthcare is at a crossroads, the Rural Health Transformation (RHT) Program is an extraordinary opportunity to reimagine care in rural communities across the U.S. Where historical support for rural health has traditionally been structured as grants or cost-based reimbursement, the RHT Program presents a rare and significant moment to catalyze dramatic transformation of care delivery in rural communities by investing in innovative technologies, sustainable access, and providers who can meet the needs of rural communities. States must act with urgency and creativity to deliver new capacity and new capabilities to their small towns and rural areas.
Established by the One Big Beautiful Bill Act (OBBA), the RHT program enables states to apply for $50 billion over five years for rural health initiatives. States must apply for the funding, and eligible initiatives include:
- Evidence-based chronic disease prevention and management
- Value-based care initiatives
- Technology-driven care solutions
- Behavioral health access
- Rural provider recruitment and retention
- Cybersecurity and health IT support
Persistent challenges in healthcare access, affordability, and outcomes have made clear that patching up legacy systems is no longer enough. Real transformation won’t come from doubling down on the status quo, nor from sourcing point solutions purely focused on technology without consideration of how it will be deployed.
The Need: Rural Health is in Crisis
Rural Americans experience worse health outcomes across nearly every measure:
- 28% of rural residents have two or more chronic diseases.1
- Preventable hospitalizations are 40% more common in rural areas.2
Those outcomes are the result of some serious challenges in primary care delivery in these areas:
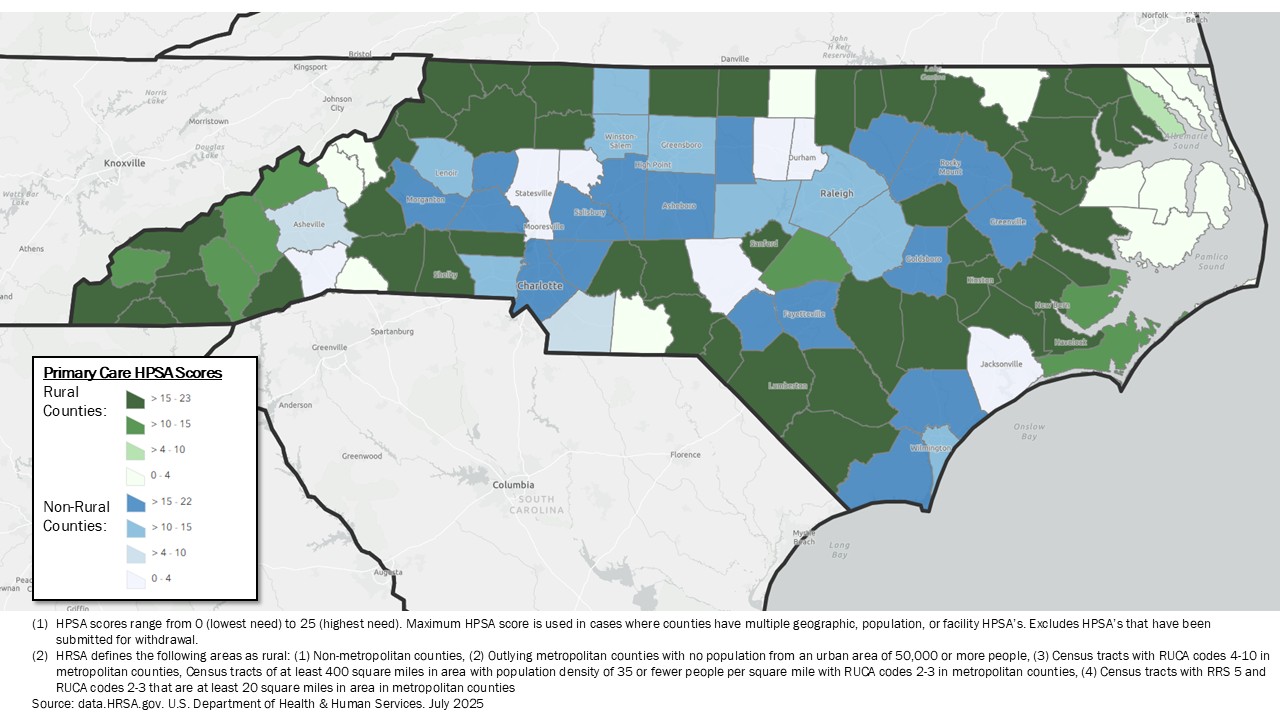
- 66% of primary care shortage areas are rural areas.3
- There are only 46 PCPs per 100K people in rural communities – compared to 61 PCPs per 100K in urban settings.4
- There are only 30 specialists per 100,000 people in rural communities – compared to 263 specialists per 100,000 in urban settings.5
Despite billions in investment, traditional infrastructure alone can’t meet the growing needs of these communities. Many rural hospitals are operating below capacity, rely too heavily on federal funding, struggle with workforce recruitment and retention, and are only equipped to focus on acute needs rather than prevention. While rural hospitals excel greatly at providing great care with the limited resources they have, they often lack the tools and resources to embrace technology-enabled innovation. With nearly 200 rural hospitals closing in the past two decades and more than 700 at risk, the need has never been greater for new partners and solutions that can strengthen care, expand access, and bring innovation closer to home.
North Carolina Primary Care Health Professional Shortage Areas
Meanwhile, emergency department utilization in rural areas is rising twice as fast as in cities – signaling a lack of access to timely, preventive, and primary care services. The crisis is hitting older and poorer populations hardest, which makes up a larger share of the population in rural areas:
- 18% of rural residents are 65 and older, compared to 14% in urban areas.6
- 15% of rural residents in rural areas live below the poverty line, compared to 12% in urban areas.7
- 24% of rural residents are covered by Medicaid, compared to 21% in urban areas.8
Without a sustainable solution that addresses the root cause of rural health challenges, rural communities will fall even further behind.
The Case for Technology-Driven Innovation
Recent advancement in new technologies, like AI-enabled care delivery tools and remote patient monitoring, have tremendous opportunity to transform rural care delivery – by reducing physician burnout, extending physician expertise, increasing access to care, and creating a better patient experience. We use these technologies every day at Hopscotch, and the RHT offers an opportunity to learn from prior efforts to deploy EMRs in rural areas and instead embrace technologies that will define the next generation of care delivery.
However, technology-driven innovation requires foundational elements – like trusted physician-patient relationships, access to reliable high-speed broadband, local clinical workforce training and recruitment programs, and access to in-person care when virtual care is insufficient. By investing in these areas, the right environment can be created for technological innovation and adoption.
Recommendation to States
Rural healthcare doesn’t need more band-aids – it needs bold transformation. State health leaders have a once-in-a-generation opportunity to think bigger and use RHT funding to build a sustainable, technology-enabled system that builds on the strength of rural communities and works better for patients, providers, and taxpayers alike.
To build a brighter future and maximize impact of the funds, we must collectively champion three critical drivers of lasting impact. It is our recommendation to state leaders to invest in the following areas:
Technology-Enabled Care Expansion: To extend care beyond the clinic, manage chronic disease, and enhance patient outcomes, states should invest in technology-enabled tools such as AI clinical decision support tools, remote patient monitoring, and telehealth. Supporting access to virtual specialty care, behavioral health services, preventive services, and early-detection screening can help fill critical gaps facing rural providers today.
Workforce Recruitment and Development: To address provider shortages and build a long-term talent pipeline, states should invest in workforce development through wage supplements, pathway programs between local training programs and rural health providers, recruitment and retention bonuses, loan forgiveness and repayment, thoughtful scope-of-practice regulations, interstate licensing compacts, and rural-focused residency programs.
Pathways to Sustainability: To ensure initiatives endure and deliver lasting impact, states should focus funding on initiatives that have viable pathways to sustainability on their own terms and on care models that effectively manage and improve quality of care, health outcomes, and health care costs. This can be enabled by prioritizing value-based care reimbursement models, encouraging collaboration across health care providers, and leveraging private capital to extend public funding.
Let’s build the future of rural healthcare – together.
About Hopscotch Primary Care
Hopscotch Primary Care is on a mission to transform lives in rural communities through accessible and proactive value-based primary care. Hopscotch serves seniors through advanced primary care clinics, led by outstanding primary care providers and enabled by best-in-class technology.
Footnotes:
- Rural Health Information Hub. “Chronic Disease in Rural America.” Rural Health Information Hub, 24 Mar. 2025.
- Johnston, Kenton J., Hefei Wen, and Karen E. Joynt Maddox. “Lack of Access to Specialists Associated with Mortality and Preventable Hospitalizations of Rural Medicare Beneficiaries.” Health Affairs, vol. 38, no. 12, 2019, pp. 1993–2002.
- Rural Health Information Hub. “Healthcare Access in Rural Communities.” Rural Health Information Hub, 17 July 2025.
- Liu, Michael, and Rishi K. Wadhera. “Primary Care Physician Supply by County-Level Characteristics, 2010–2019.” JAMA, vol. 328, no. 19, 15 Nov. 2022, pp. 1974–1977.
- National Rural Health Association. “About Rural Health Care.” National Rural Health Association, n.d.
- Cohen, Steven A., and Mary L. Greaney. “Aging in Rural Communities.” Current Epidemiology Reports, vol. 10, no. 1, 2023, pp. 1–16.
- Economic Research Service, U.S. Department of Agriculture. “Rural Poverty & WellBeing.” U.S. Department of Agriculture Economic Research Service, 14 Jan. 2025.
- Euhus, Rhiannon, et al. “5 Key Facts About Medicaid Coverage for People Living in Rural Areas.” KFF, 26 June 2025.